There was a crew of labourers on my construction site who went hard. This crew was in charge of stripping the wooden forms (a kind of mould used in construction) off the newly poured concrete, a task that involved holding massive metal scrapers and crowbars above their heads and hacking at the wood on the ceiling until it peeled away. The work was hard and dangerous — the new guy fell off the side of the building, saved only by his safety harness and lanyard. They were fast, though. Fast is good: fast means you won’t get laid off and replaced. Fast means money.
I found out that some of them did cocaine and speed to keep up the energy necessary to do the work. But they would also pull muscles in their arms and back and injure themselves. Some of them would smoke weed on the site, or more potent forms of THC like Shatter. They would go to the clubs on weekends and get high — partly for fun, partly to keep themselves awake after weeks of exhausting manual labour.
My friends, the labourers, moved on to Percocet, OxyContin and other opioids. One day I saw my friend up on the slab, his eyes dilated, barely keeping it together. I whispered to him he should find some excuse to get down on the ground, that he was way too high to keep working. He said he had to keep working or he’d get laid off. But as the site wound down, even before the concrete formwork was finished, he got laid off anyway. He and the team he’d assembled had worked themselves out of a job, plus the rumours of drug use were getting too much for the foreman. Now my friend was a liability.
Scenes like this play out on construction sites around the country every day. Workers dealing with workplace injuries, precarious work, stressful work environments and abuse at work often use drugs and alcohol to cope. The stigma around drugs makes it hard to talk about or address the problem, or even measure it. But there is one statistic we can measure: Construction workers have the highest rate of death by overdose of any group of employed people — representing one third of deaths among all employed people in Ontario, and one fifth of total deaths in British Columbia.
Overdoses and lethal overdoses are increasing across the country, due in part to the social isolation and stress of the pandemic, and the increasing amount of more powerful and faster-acting synthetic opioids such as fentanyl and carfentanil. From 2019 to 2021, overdose deaths increased by 66 per cent. British Columbia, Alberta and Ontario have been hit especially hard, but other provinces are also seeing increased deaths, with 87 per cent of opioid-toxicity deaths fentanyl-related. If we don’t address the link between this phenomenon and the construction industry, and develop plans with unions and workers that address the specific needs of workers who use drugs, the human toll will continue to rise.
Workers in Pain
The subject of pain comes up again and again in my interviews with construction workers. They face repetitive strain injuries and dangerous workplace environments. Even unionized construction workers deal with extremely precarious and often short-term worksites, from which they can be laid off at any time. Construction workers are not paid for time off, and traumatic injuries are common.
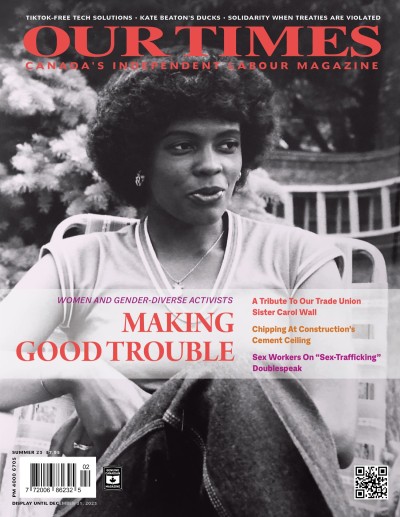
PHOTO-ILLUSTRATIONS: BARBARA BAILEY. SOURCE IMAGES: ISTOCK.
“Tony” (some names have been changed to protect these interviewees’ identities) had an opioid addiction for 27 years and works as a gig worker in construction, among other industries. He says, “There’s a lot of people on the job site who are into drugs. Probably because they suffer from a lot of pain and can only get so much pain relief.” He adds that people dealing with addictions often work in construction. “Think about it: drugs are expensive. People who use hard drugs, who are able to use hard drugs, have to have a job, whether it be in the film industry, the carpenters, day labourers, whatever.”
“Max” is a sprinkler fitter from Vancouver, working on large sites. He says, “I think people in all industries use opioids. I do know that within construction there is a culture of working with pain and injury without talking about it. People need a paycheque so they go to work however they can. This makes me suspect that a lot of workers use opioids as pain relief on a regular basis while at work. I personally use opioids as pain relief at work occasionally.”
“Vince” works in non-union residential construction. He says “Vitamin P” (Percocet) is ubiquitous at work. “In the drywall life, when it takes all hands to take drywall to the third floor, I’m off with Vitamin P that gets me through the day,” he says. “There are guys taking six a day and are functioning. You might get offered one by the boss, but they aren’t a doctor. They say this will help through the day, or take a half of these. But there is zero tolerance for intoxication at work: [the dose] is either matching their pain or matching their level of addiction.”
Cindy Krysac is an IBEW-unionized electrician and mental health advocate. Krysac has worked inside and outside the industry to create construction-specific mental health first-aid training. “Mental health problems and substance-use problems go hand in hand,” she says. “Factors are: construction is a male-dominated industry. Men are less likely to reach out for help for mental health problems (and even physical health problems). So, because it’s male-dominated, you see a reflection in the numbers of people from the industry reporting mental health problems. The construction industry has a larger representation of suicides than outside the industry. Sources say about three times the average.”
PHOTO-ILLUSTRATIONS: BARBARA BAILEY. SOURCE IMAGES: ISTOCK.
Women are heavily outnumbered in construction trades, representing less than 10 per cent and in many cases less than 1 per cent of workers (depending on the specific trade and the province). Women and non-binary workers in such a marginalized situation are not immune to toxic masculinity. Krysac says, “It’s not just about men in construction. It turns out that with women in this male-dominated industry, you see a decrease in women reaching out for help, and an increase in suicide.”
Addiction and mental health are inextricably linked. Galen, who is using his first name only for this story, is a construction electrician who has had his own struggles with drugs and alcohol and is now in recovery. He points to toxic masculinity as a root of mental health and addiction problems in the trades. He says, “I’m a recovering addict. I’m a person who has gone to therapy and dealt with a lot of the traumas that drove me to addiction, which were [from] the patriarchal organization of our society.”
“The EpiPen for Opioids”
Mark Barnes has attended a lot of construction safety meetings. He says that he’s probably “the only pharmacist in the country with work boots and a hard hat.” He does it because he’s a co-owner of Respect Rx group of pharmacies and a “passionate advocate for overdose prevention.”
He explains that anyone can carry and learn to use naloxone, especially the nasal spray, “a life-saving tool for you to help somebody.” He calls it an EpiPen for opioids, explaining, “Just like an EpiPen cannot remove peanuts from the body, it does not remove the opioids, but what it does is block the opioids from the brain centres. It reactivates the breathing until paramedics get there. You put a spray in the nose and it can only take two to three minutes to start working. You can provide the tools for them to breathe. And because most people die within three to five minutes, they can actually stay breathing until the paramedics come to save them. It’s one of the safest things a pharmacist can dispense in the pharmacy because it has zero effects on someone who has not taken an opioid.”
But naloxone is not a standard part of construction first aid kits, nor is it often talked about as part of workplace safety in the industry. Construction workers often work in remote areas, in highrise buildings, or in new buildings that aren’t on any maps yet, delaying first responders in the event of an emergency. Max says it is important to have kits at the actual worksites where people are. “Most construction sites, it takes ages to get anywhere. Paramedics need to be shown where to go and sometimes people are in hard-to-reach places, especially if they are trying to not be seen while using drugs. Right now, people need to hide it so much that I think it is not super likely to find someone on time who is overdosing. But having the kits on site is an important step towards changing that.”
Barnes’ organization is doing work specifically with the construction industry, especially in the Ottawa region. Naloxone is free in Ontario and for certain groups nationally (Indigenous Peoples and veterans), and is available at pharmacies or through public health. You can learn how to use naloxone by doing a quick training session at a pharmacy in Ontario, or by watching a four-minute video available online at Barnes’ website, naloxonecare.com. “Naloxone,” Barnes emphasizes, “is a fantastic addition to any first aid kit in Canada.”
Kim McKinnon of Toronto Paramedic Services says, “We support harm reduction. Anything that supports reducing the risk at the site would be something we would support. Toronto Public Health is offering kits; you can go into Shoppers Drug Mart and get a kit.”
Until naloxone becomes a standard part of first aid kits, workers can get their own kits and carry them themselves. Galen says, “I think that should be a fundamental part of our apprenticeship: We should teach all our members how to use naloxone. What it’s for, why we use it. It should be an essential part of our health-and-safety courses.” Tony says, “I’ve used naloxone to save people. Probably on every job site there should be a sharps box and naloxone, on every floor.”
Different Workers Need Different Approaches
“Abstinence approaches literally kill people. Overdoses are killing so many people,” says Max. “It is heartbreaking, and it is critical that we do something. As long as construction workers need to hide drug use, people will do their drugs alone, often filled with shame about it, and will be much more likely to die. And even if someone does want to cut down or stop using drugs, the stigma and fear of losing work or getting fired will keep people from accessing any supports around detoxing or quitting. This can kill people too.”
Jordan Westfall co-founded the Canadian Association for Safe Supply. He says, “I think [seeing] how heavily impacted the trades, specifically construction, have been from the overdose crisis, we need interventions that are focused on them and tailored to them. It’s often hard for those with jobs to access harm-reduction services — fear of stigma, fear of discipline at work, etc.”
Tony says, “It’s almost easier to stay on drugs than to get into treatment. Plus, when you’re in treatment the whole fucking job place knows you’re on Dope. I would say to someone in that situation, obviously, go get help. But it’s really hard. There is such a stigma about it. Let’s say you need to go see a doctor on a Wednesday afternoon, and it’s once every couple of weeks. The foreman is gonna start noticing. So, either you bullshit them or you tell them the truth, and what happens when you tell the truth? That you have an opiate problem or an addiction problem? What are they gonna do when it comes to that?”
Construction unions in Toronto fund a rehab centre, with a five-week program that includes possible referrals to special programs elsewhere. Karen Pullen is an executive member of IBEW Local 353 and does intake for members who need rehab. “There has been a huge influx, but there always have been issues in this field,” she says. “Years ago, in the ’80s, Ontario building trades started the De Novo Centre because the need was so great. It’s always been that construction workers are higher on the [list of those who] need addictions help.”
The fact that the treatment centre can be accessed through the union is especially helpful, and people can do an intake with the union without necessarily involving their own work supervisors. Elaborating on her own role, Pullen says, “As a rep, I can help our members keep their job by facilitating a return-to-work agreement with contractors.” In her experience, they are often supportive. “I have found most contractors are willing to do what they can to help employees regain a stable life.”
PHOTO-ILLUSTRATIONS: BARBARA BAILEY. SOURCE IMAGES: ISTOCK.
“Abstinence is great for some, and going away to rehab is great,” says Barnes. “But eventually, you gotta get well in your own environment, in your own stressful life. Give a person a lower-risk alternative [to find] wellness . . . harm reduction is what works. As health professionals, we have to start talking and take a different look at this.”
Treatment options can be difficult for people to access because of their work schedule. “Methadone and the workplace is pretty hard to do,” says Tony. “If you’re still using every day, it’s gonna be a hassle. Because eight o’clock is when the pharmacy opens, and if you’re still using, you’re fucked.”
Barnes’ pharmaceutical organization has been working to make harm reduction tools more accessible to construction workers, by, for instance, opening their doors at 6:30 in the morning to provide treatment. Barnes’ team also discovered that people working physical labour — especially in the summer — need higher doses of methadone or other harm-reduction drugs than people who do more sedentary work, because their metabolism increases while they’re working. This is the type of industry-specific consideration that needs to happen if addiction issues in the construction industry are to be effectively addressed.
Tony says that the programs in place for take-home treatment options that don’t require daily pharmacy visits, known as “carries,” require very frequent visits to a doctor at first, which he says make it “really hard to maintain employment. The whole opioid program is kind of fucked up because you have to go every day if you’re using. I don’t have that problem. I can go to work every day and I haven’t used drugs in like 10 years.”
Westfall, based in BC, agrees with Tony’s analysis. “It’s very common in each province that people can’t receive carries, or only receive them once they’ve been in a program for a certain length of time,” he says. “Programs need to be flexible enough so that people can continue to live their lives. Going to a clinic every day is difficult for most people.” He adds, “We really need to let people get take-home carries of safe-supply drugs or OST (opioid substitution therapy).”
Westfall mostly works on “safe supply,” a term he coined. “The need for safe supply has grown with the fentanyl crisis,” he says. “We know from the evidence that abstinence-based treatment is not successful for many people. Worse, going in and out of treatment can actually increase overdose risk. People leave treatment when their tolerance for drugs is down, and if they use they’re at a greater risk of overdose. Also, there are people who want to use drugs for whatever reason, and rehab is a non-starter with them. If we don’t give them an alternative to the illicit supply, and they also refuse treatment, we will see more overdose deaths needlessly.”
Most pharmacists, including advocates like Barnes, prefer the term “safer supply.” He has been rolling out programs in the Ottawa region. In BC, Westfall says, “some pharmaceutical options for people, specifically hydromorphone tablets” are being introduced. “However, these measures have only gotten a few thousand people prescribed drug access.” He says that the provinces, in general, are not doing enough to support safe-supply pilot projects, which have been relying on federal funds, even though health is a provincial responsibility.
Whatever plans are developed need to look at how construction workers are disproportionately affected by the opioid overdose crisis, and how these same workers have specific access needs that require customized solutions. As Galen says, “Like anything that seeks to alleviate or fix problems that have to do with human beings, there is no blanket solution here.”
Megan Kinch is a labour journalist and a working construction electrician, unionized with the IBEW. Her work has been published in Briarpatch, Spacing, Today’s Parent, This, NOW and Midnight Sun, on CBC, and by Equal Times and the Canadian Labour Institute, among others. Follow her @meganysta on Twitter.